In today’s evolving landscape of diagnostic medicine, the integration of complementary imaging technologies is redefining how clinicians detect, assess, and monitor disease. Two non-invasive modalities—medical-grade thermography and diagnostic ultrasound—have individually proven their worth in clinical settings. Yet, when these tools are combined, their collective diagnostic power offers a more comprehensive understanding of physiological and anatomical conditions, enhancing the accuracy and effectiveness of patient care.
This article highlights the valuable alliance between thermography and ultrasound imaging, illustrating how thermography’s functional, heat-based data guides targeted, structural evaluation through ultrasound. Additionally, we explore how Doppler ultrasound’s capability to assess vascular patterns aligns with thermographic readings, offering a dynamic, multi-dimensional perspective of pathology. Together, these technologies support early detection, monitoring, and integrative care strategies across a range of clinical applications.
Thermography: Capturing the Body’s Thermal Signals
Medical thermography operates by detecting and mapping infrared heat emissions from the body’s surface. Because changes in circulation, inflammation, and nerve activity affect skin temperature, thermography can identify subtle physiological changes that may indicate developing disease, often before structural abnormalities are detectable by other imaging modalities.
Widely known for its role in breast health assessments, thermography is valued for its radiation-free, non-invasive nature and its capacity to detect abnormal heat patterns related to increased vascular activity or inflammation. Beyond breast imaging, thermography is increasingly applied in vascular screening (such as carotid artery assessments), thyroid dysfunction evaluations, and musculoskeletal and nerve-related conditions.
Primary advantages of thermography include:
* Detection of early physiological changes that precede structural issues.
* Non-invasive, radiation-free imaging suitable for regular monitoring.
* Identification of heat patterns associated with abnormal vascularity, inflammation, or nerve irritation.
* Ability to perform comparative, sequential imaging to monitor physiological trends over time.
Although thermography is not intended to replace anatomical imaging, its sensitivity to functional abnormalities makes it a valuable tool in proactive and complementary diagnostics.
Ultrasound Imaging: Anatomical Insight and Dynamic Evaluation
Diagnostic ultrasound uses high-frequency sound waves to create real-time images of internal tissues and structures. Its versatility allows clinicians to visualize soft tissue anatomy while also assessing movement and blood flow using Doppler technology.
Ultrasound is routinely used for evaluating breast, thyroid, vascular, abdominal, pelvic, and musculoskeletal health, among other applications. Doppler ultrasound adds a critical dimension by enabling clinicians to observe blood flow patterns, vessel integrity, and abnormal vascular activity such as tumor angiogenesis or inflammatory hyperemia.
Notable strengths of ultrasound imaging include:
* Immediate, real-time visualization of anatomical structures.
* Functional assessment of blood flow with Doppler imaging.
* Safe, non-invasive, and adaptable for various anatomical regions.
* Guidance for needle biopsies and interventional procedures.
Ultrasound’s ability to combine structural detail with dynamic functional data makes it an ideal counterpart to the physiological information captured through thermography.
Thermography as a Guide for Targeted Ultrasound Evaluation
The value of pairing thermography with ultrasound lies in how thermal imaging can direct more precise, focused ultrasound assessments. Thermography highlights areas of abnormal heat distribution, which often correspond to regions of increased blood flow, inflammation, or nerve activity beneath the skin. These thermal findings can then inform where ultrasound should be applied, ensuring that subclinical or early-stage concerns are investigated further.
In clinical scenarios such as:
* Breast health assessments: A localized heat anomaly on thermography may indicate increased vascular activity. Focused ultrasound imaging, supplemented with Doppler studies, can then examine the area for masses or abnormal vascularity.
* Carotid artery evaluation: Thermal asymmetries along the neck may signal vascular irregularities or inflammation. Doppler ultrasound can assess blood flow velocities and vessel patency at these flagged locations.
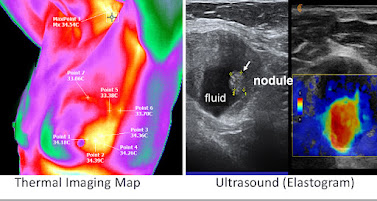
* Thyroid screening: Thermal patterns suggestive of hyperactivity or inflammation can prompt targeted ultrasound evaluation to visualize nodules, cysts, or vascular changes.
This coordinated approach improves diagnostic accuracy by combining thermography’s sensitivity to functional changes with ultrasound’s structural and functional imaging capabilities.
Aligning Vascular Data: Doppler Ultrasound Meets Thermography
Doppler ultrasound’s role in measuring blood flow dynamics aligns naturally with the vascular insights offered by thermography. Both modalities offer distinct, yet complementary, information about circulation and tissue metabolism.
For example:
* Tumor-related angiogenesis often results in increased local blood flow, creating areas of hyperthermia on thermography and detectable vascular proliferation with Doppler ultrasound.
* Inflammatory processes generate heat due to increased blood flow and metabolic activity. Thermography can map these hotspots, while Doppler ultrasound confirms hyperemia and assesses the involved vessels.
* Peripheral vascular disease may appear as cooler regions on thermography due to impaired perfusion. Doppler ultrasound can then quantify blood flow reduction or identify vascular obstructions.
* The alignment of these two data sets provides clinicians with a thorough understanding of both functional vascular health and anatomical vessel status.
Broadened Applications: Established and Investigational Uses
While thermography holds FDA clearance as an adjunct for breast health evaluation, practitioners have extended its use into several investigational areas where early physiological changes are clinically relevant.
Examples include:
* Neuropathy and pain syndromes: Thermography can detect altered heat patterns associated with nerve irritation or dysfunction in the back, feet, and pelvic areas.
* Inflammatory arthritis and rheumatic conditions: Localized heat increases can identify active inflammation sites.
* Post-surgical surveillance: Thermography may help track vascular integrity and inflammation following operative procedures.
* Sports injuries and overuse syndromes: Subtle thermal changes can signal early-stage tissue stress or inflammation, while ultrasound evaluates tissue integrity and guides treatment.
In each scenario, ultrasound enhances the diagnostic process by confirming structural pathology or assessing blood flow in areas identified by thermography, allowing for more precise intervention planning.
Illustrative Example: Integrating Imaging for Breast Health
Consider a clinical case in which thermography reveals a localized area of elevated heat in the upper outer quadrant of the left breast. This finding prompts a targeted ultrasound examination, which identifies a small, hypoechoic mass with notable vascularity on Doppler imaging. The combined results offer a compelling clinical rationale for further investigation, such as biopsy or additional imaging.
In situations where breast tissue density limits mammographic accuracy, thermography and ultrasound together improve the likelihood of early detection, providing valuable information in risk assessment and management planning.
Conclusion: A Forward-Thinking Diagnostic Model
The combined use of medical thermography and ultrasound imaging represents a progressive, integrative model in diagnostic medicine. By coupling physiological heat mapping with real-time anatomical and vascular imaging, clinicians can detect early, often subclinical changes that may signal the onset of disease. This dual-modality approach offers a safer, non-invasive, and highly informative option for proactive health monitoring and early intervention.
As diagnostic medicine continues to evolve, the partnership between thermography and ultrasound promises to play an increasingly significant role, particularly in breast health, vascular screening, thyroid evaluation, and investigational applications in pain, inflammation, and sports medicine. Future research and clinical protocols will further refine and expand these applications, advancing the goal of truly personalized, precision-based care.
__________________________________________________________________________________
RELATED ARTICLES
ADVANCED THERMOLOGY FOR THYROID AND CERVICAL DIAGNOSTIC EVALUATION
THE THYROID GLAND, situated anteriorly in the lower neck, is uniquely accessible due to its superficial anatomical position and rich vascular network. This makes it an ideal candidate for assessment through high-resolution infrared thermographic imaging. Thermology offers a non-invasive, radiation-free adjunctive modality that complements traditional diagnostic methods in evaluating thyroid function and pathology. By detecting subtle temperature variations on the skin surface above the thyroid and surrounding cervical tissues, infrared thermography reflects the gland’s underlying metabolic activity. This technique is especially valuable in the early detection and functional assessment of thyroid disorders, including Hashimoto’s thyroiditis, Graves’ disease, nodular goiter, and thyroid malignancies.THE ROLE OF NEOANGIOGENESIS IN BREAST CANCER DETECTION
One of the core principles of medical thermography is detecting physiologic changes associated with cancer. Neoangiogenesis—the formation of new blood vessels—is critical for tumor growth. Without it, cancerous cells would be unable to obtain the nutrients they need to proliferate. The abnormal structure of these new blood vessels was not well understood until the late 1980s, when studies revealed their unique porous nature.Unlike normal blood vessels, which have a structured, three-layered composition, neoangiogenic vessels are disorganized and resemble a natural sponge, with an erratic, unregulated flow. Lacking smooth muscle and autonomic nervous system regulation, these vessels exhibit excessive and uncontrolled blood flow. As a result, areas of neoangiogenesis appear as "hot spots" in thermal imaging. Because breast tissue is located in the outer shell of the body, where body heat is regulated to maintain a stable core body temperature, these hot patterns can indicate malignancy, setting medical thermology apart as a functional imaging modality distinct from structural imaging techniques like mammography, ultrasound and MRI.
----------------------------------------------------------------------------------------------------------------------
HEAD AND NECK: QUANTITATIVE THERMAL MEASUREMENT & A MEDICAL COMPLETEMENT TO THE ULTRASOUND
The patient is a 65-year-old military veteran who sustained a fall, leading to a concussion that required a three-day hospital observation period. Upon discharge, he reported persistent shoulder pain. Ultrasound imaging of the shoulder revealed an inflamed biceps tendon, which was appropriately treated with physical therapy or targeted injection—avoiding unnecessary rotator cuff surgery, which had initially been planned. Given the patient’s recent concussion, ultrasound assessment was extended to the optic nerve, which was imaged within minutes and confirmed as normal, ruling out increased intracranial pressure.Optic nerve swelling is also another a critical indicator of elevated intracranial pressure and is widely used in emergency medicine for concussion assessment. While hospital concussion screenings may clear a patient, they do not eliminate the risk of delayed-onset intracranial bleeding. Subdural hematomas, for example, can develop over days, weeks, or even months post-injury, gradually increasing intracranial pressure. Early detection using noninvasive imaging techniques is therefore essential and timely.